Patients continually indicate that their ideal clinician is one who listens. At the same time, the complaint that “doctors do not listen” is ubiquitous. This webinar explores this apparent paradox by addressing what listening actually is in clinical settings, its importance and impact and whether listening can be taught and learned.
During this webinar, Dr. Fuks teaches us what listening is in clinical settings and its function in clinical interactions, as well as why listening is the foundation of the clinical method. He also explains the different types of “deafness” found among caregivers and their causes. Finally, he instructs us how to teach clinical listening skills.
How a clinician behaves through nonverbal signals and style has an impact on patients and is considered an important component of patient-centeredness. Similarly, the clinician’s skills in accurately perceiving the patient (for example, the patient’s emotions, health experiences, needs, expectations or personality) are important for diagnosis, decision making and creating a wholesome relationship. Nonverbal skills can be improved through practice, insight and training interventions.
During this webinar, Judith discusses the importance of nonverbal communication in clinical and personal interactions, and reviews the supporting research evidence from social psychology and medicine. Tips from this webinar can be used for improving interpersonal perception skills in clinical situations.

Life is constantly changing. And life in health care is changing at an unprecedented pace. Sharon Salzberg, meditation teacher and renowned author, teaches us that in the midst of such change, there is not only uncertainty but also endless possibility and movement. To the question, “Can compassion be learned?” she responds with a resounding, “Yes!” Sometimes, all it takes is truly paying attention to the people around us. By paying attention to our experiences with sensitivity, we open our minds and our hearts, and understand how our actions affect others.
During this webinar, Sharon teaches us balanced ways of paying attention as a gateway to compassion. She explains the distinctions between empathy and compassion and why compassion for self and others is important in preventing burnout. Finally, she invites participants to experience a brief, secular compassion meditation as a method of transforming our worldview into one that acknowledges our fundamental connectedness.
Want to learn more about how to care for your patients and their families while taking care of yourself? View Dr. Beth Lown’s webinar, the first in our monthly webinar series on the concepts and skills you need to thrive in today’s health care environment.
Dr. Lown will introduce a framework of essential skills that put compassion and collaboration into practice and help you relate to patients, families and your coworkers more effectively. She’ll discuss some of the exciting new research on compassion, which demonstrates that we can learn to improve these essential skills, and she’ll talk about how compassion can help prevent burnout.
It would be beneficial to watch this webinar for context before watching the others in this series. Each monthly webinar will highlight one of the skills introduced in this session.
Family meetings are a routine part of care for seriously ill patients and their families. Effective conduct of these meetings has been associated with improved patient care and improved family outcomes. In this webinar, Dr. Curtis shares tips for both running and teaching positive family meetings, improving interdisciplinary communication, facilitating shared decision making around end-of-life care and how to use family meetings as a quality measure.
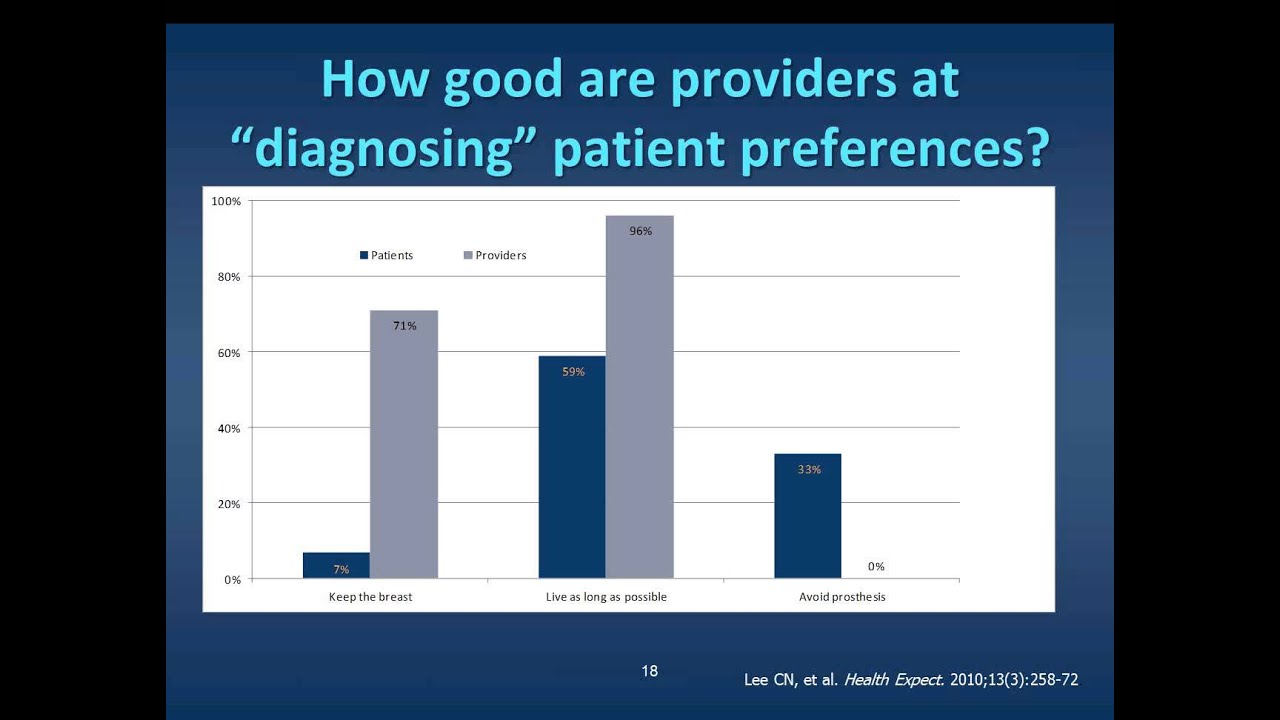
Everyone talks about shared decision-making, but most clinicians have not been trained in the specific communication skills required. To provide true patient-centered care, providers must probe to understand the patient’s unique circumstances, values, and preferences in order to help arrive at a therapeutic choice that fits his/her individual needs. This webinar reviews how to elicit patient preferences, how to communicate risks and benefits effectively, and how to recognize and help patients resolve decisional conflict.

Carol reviewed the RESPECT model, and how caregivers can use it in their daily practice, teaching and supervision. A relational model that addresses difference and power, RESPECT identifies skills to build trust with patients, especially with those who differ from the caregiver by race, culture or background. It is a helpful training tool that also guides preceptors and supervisors to partner with learners, supervisees and colleagues across differences in hierarchy. This webinar includes educational tools for observing, communicating and supervising with RESPECT. New work using RESPECT to address diversity and hierarchy on multidisciplinary teams is also highlighted.

Dr. Jackson addresses the myths and barriers associated with communicating challenging information to patients and present a cognitive model for prognostic disclosure. Viewers will gain a deeper understanding of the research supporting different communication strategies for discussing difficult content and addressing patient and caregiver emotions.
Compassionate care is critical but often an underutilized component in improving patient outcomes and reducing professional liability exposures. At its core, it means treating patients in a holistic manner, rather than focusing only upon patient illness. A growing body of research demonstrates that patient-centered care is essential to quality healthcare and has been associated with improved health outcomes, increased patient satisfaction, better adherence to treatment recommendations and fewer medical errors and malpractice claims.
© 2025 The Schwartz Center. All Rights Reserved.